While we continue to improve our oral health from generation to generation, we’re not disease-free quite yet. It’s true that advances in patient education, publicly available aids like fluoridated tap water, and new and more affordable technologies have reduced instances of tooth decay in the United States. But gum disease is still a significant problem. In fact, the CDC estimated that between 2009-2010, one out of every two Americans age 30 and up had periodontal disease. This includes any form of periodontal disease, whether mild or severe, but it’s still a discouraging number.
Since gum disease is the primary cause of tooth loss, it’s especially important to stay vigilant if you’re interested in keeping your smile intact (and who isn’t?). Fortunately, if you catch gingivitis early, treatment is simple and many patients can actually reverse gingivitis at home. You just need the necessary education so that you can keep an eye on your gums and react when something begins to change for the worse. We’ve put together everything you need to know about periodontal disease below. And while home care is crucial, you need to back that up with regular exams – schedule yours today.
Gum Disease Risk Factors
There are certain factors that make you more likely to experience gum disease at some point in your life. While some of these are unavoidable, many are preventable. If you’re at a high risk based on your family background, it’s wise to be extra careful with your habits and oral hygiene.
Consider your own background to determine whether any of the following might apply:
- Family history of gum disease
- Tobacco use of any kind
- Conditions that are linked to gum disease, like diabetes, arthritis, and heart disease
- Being over the age of 65 (over 70% of Americans in this age group have gum disease)
- Being male (men are more likely than women to develop gum disease, although this may be linked to their increased use of tobacco and alcohol)
- Certain medications that cause dry mouth
- Compromised immune system
- Poor nutrition
- Chronic teeth grinding, which causes gum recession and potential irritation
How to Spot Gingivitis Before It Progresses
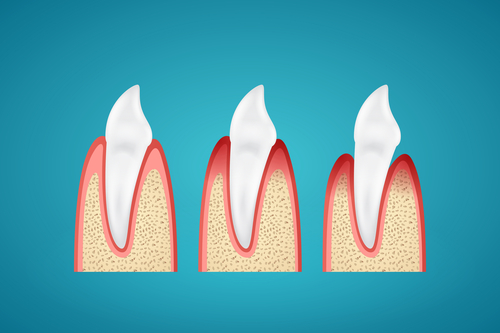
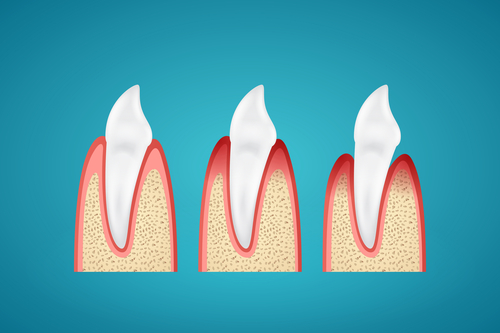
Gingivitis is the first stage of periodontal disease. At this point, plaque buildup on the teeth has begun to irritate the gum line. When plaque builds up, the bacteria involved release acids that harm the gums. The gums react by becoming inflamed. This is the most noticeable component of gingivitis – but that’s not all you can look for.
Something that’s always important to remember is that each patient experiences gingivitis differently. In some cases, symptoms might not be visible to the untrained eye. This is just one reason why we recommend scheduling regular exams. Most patients benefit from visiting their dentist every six months. If you’re in a number of high risk categories, you may benefit from more frequent exams.
In between your appointments, be aware of the following:
- Swollen gums – When our bodies fight off infection, the area with excessive bacteria typically becomes inflamed. This happens because the body is attempting to isolate the bacteria responsible for the infection and keep it from spreading.
- Gums that bleed easily – Your gums only bleed for a few reasons. One, you had some kind of soft tissue injury. Two, you just started flossing for the first time and your gums are sensitive (keep at it – the bleeding and sensitivity will soon fade). Three, the gums are irritated from plaque buildup and developing gingivitis. If your gums have just started bleeding out of nowhere, it’s a good idea to check in with your dentist.
- Dark red or purple gums – This discoloration may appear at the edges of your gums, where the teeth and gums meet. This is also a sign of the body fighting infection. If your gums are looking deep red or purplish, you may have gingivitis.
- Bad breath – If no amount of brushing or flossing is improving your breath, periodontal disease is a potential culprit. Excess bacteria in the mouth can worsen your breath and keep it less than fresh. This may also present as a bad taste in the mouth.
- Gum recession – Irritated gums may recede, pulling away from your teeth and exposing tooth roots. This is also a symptom of teeth grinding, which is also something you should check on with your dentist.
Improving Gum Health at Home
- Start flossing – If you have plaque buildup and are experiencing gingivitis as a result, kickstarting your oral hygiene will help you remove plaque and get back to normal. If you’re not currently flossing, picking up the floss will help make a difference. Floss accesses areas that toothbrushes can’t, especially if you have crowded teeth.
- Use mouthwash – An antibacterial mouthwash will help treat gingivitis by removing bad bacteria from the mouth. Look for one with the ADA’s seal of approval, or ask us for a recommendation.
- Get more consistent with your oral hygiene – Make sure you’re brushing at least twice daily and flossing once daily. If you tend to forget before you go to sleep, put a reminder on the mirror or on your phone.
- Drink plenty of water – Water helps reset your oral pH and rinse away harmful bacteria. Plus, it’s great for your whole body!
Dalton General Dentist | General Dentistry Dalton | General Dentist Dalton